Post-Traumatic Stress Disorder (PTSD) is a significant problem for veterans of the wars in Iraq and Afghanistan. A large number of military personnel have presented with combat-related trauma, and the veterans of these conflicts have been exposed to operational stressors that differ from those of previous wars. As a result, ensuring effective treatment of afflicted service members has become a priority.
PTSD is a disabling anxiety disorder that emerges after an acutely distressing event of a terrifying or catastrophic nature. The core symptoms of the disorder are persistent re-experiencing of the trauma, avoidance of trauma-related stimuli, negative alterations in cognitions and mood, and increased arousal and reactivity. Military personnel, especially those directly involved in combat operations, are at an increased risk of developing the disorder.
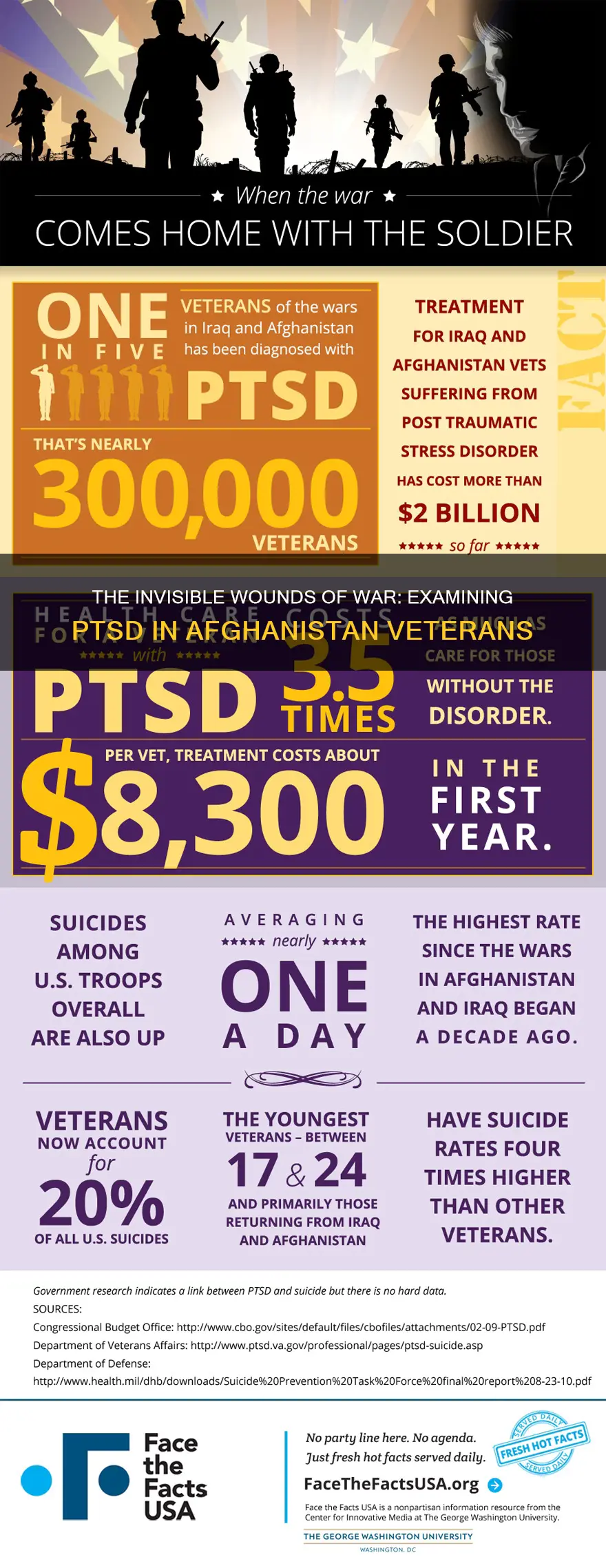
Estimates of the prevalence of PTSD among service members vary between studies. An observational study of over 18,000 US Army soldiers returning from Iraq and Afghanistan described the self-reported prevalence of PTSD to be 15%. Similarly, a comprehensive study of the prevalence of this disorder among over 13,000 veterans deployed during OEF/OIF indicated an overall rate of 15.8%. An extensive meta-analysis estimated a prevalence of 12% among combat units and 5% among non-combat units. Although estimates vary, the research literature indicates that veterans in general, and combat veterans in particular, are at a much greater risk of being diagnosed with PTSD than civilians.
PTSD is a significant public health problem in Operation Enduring Freedom and Operation Iraqi Freedom (OEF/OIF) deployed and non-deployed veterans and should not be considered an outcome solely related to deployment. A study found that 15.7% of OEF/OIF deployed veterans screened positive for PTSD compared to 10.9% of non-deployed veterans. Overall, 13.5% of study participants screened positive for PTSD.
The troubling news and images emerging from Afghanistan as American troops withdraw from the region after 20 years is causing a spike in post-traumatic stress among veterans at home. As many as 40% of service members are affected by PTSD, according to one psychiatrist. The condition affects not only those who served in Afghanistan but also those who served in Iraq and Vietnam.
| Characteristics | Values |
|---|---|
| PTSD rate among Afghanistan veterans | 7.1% |
| PTSD rate among Iraq veterans | 12.9% |
| PTSD rate among veterans deployed to both Iraq and Afghanistan | 10.4% |
| PTSD rate among veterans deployed to Iraq or Afghanistan | 10.9% |
| PTSD rate among veterans | 13.5% |
| PTSD rate among deployed veterans | 15.7% |
| PTSD rate among non-deployed veterans | 10.9% |
| PTSD rate among deployed male veterans | 16.2% |
| PTSD rate among non-deployed male veterans | 10.5% |
| PTSD rate among deployed female veterans | 12.5% |
| PTSD rate among non-deployed female veterans | 12.3% |
What You'll Learn

Prevalence of PTSD among Afghanistan veterans
The prevalence of PTSD among Afghanistan veterans has been a growing concern for mental health professionals. The condition affects as many as 40% of service members, with the condition being more prevalent among those who have been deployed to conflict zones.
PTSD among Afghanistan veterans
A study of over 18,000 US Army soldiers returning from Iraq and Afghanistan found that the self-reported prevalence of PTSD was 15%. Another comprehensive study of over 13,000 veterans deployed during OEF/OIF indicated an overall rate of 15.8%. An extensive meta-analysis estimated a prevalence of 12% among combat units and 5% among non-combat units.
Factors influencing PTSD prevalence
Several factors can influence the prevalence of PTSD among Afghanistan veterans. These include the intensity of combat, multiple deployments, and the use of prescription medications and substance misuse to cope with the aftermath of trauma. The recent withdrawal of American troops from Afghanistan has also triggered post-traumatic stress among veterans, causing a spike in cases.
Treatment and relapse
The standard treatment for PTSD involves psychotherapy, such as cognitive processing therapy and exposure therapy. However, there is a high rate of dropout from treatment, with estimates ranging from 36% to 60%. Additionally, there is a lack of long-term follow-up in many cases, making it difficult to determine the true relapse rate.
Impact on veterans and society
PTSD among Afghanistan veterans has far-reaching consequences. It affects not only the veterans themselves but also their families and society as a whole. The condition is associated with substance abuse, depression, interpersonal difficulties, and suicidality. It can also lead to functional impairment, affecting the veteran's ability to maintain employment, housing, and relationships.
In conclusion, PTSD is a significant issue among Afghanistan veterans, with a prevalence estimated to be higher than in the general population. Effective treatment and support are crucial to helping veterans manage their symptoms and improve their quality of life. Further research is needed to develop more robust methods of relapse detection and prevention and to improve long-term treatment outcomes.
A World Away: The Long Haul from Virginia to Afghanistan
You may want to see also

PTSD treatment programs for Afghanistan veterans
Overview
The US Department of Veterans Affairs (VA) offers a range of treatment programs for Afghanistan veterans suffering from Post-Traumatic Stress Disorder (PTSD). PTSD is a significant public health problem among veterans, and effective treatments are available.
Types of Treatment
PTSD treatments can be broadly categorized into non-pharmacological and pharmacological approaches.
Non-Pharmacological Treatment
Cognitive Behavioral Therapy (CBT) is considered a first-line approach and is recommended in PTSD practice guidelines worldwide. Two of the most studied types of CBT are Cognitive Processing Therapy (CPT) and Prolonged Exposure (PE) therapy. CPT focuses on helping patients identify and replace negative thoughts related to the traumatic event, while PE therapy involves repeated revisiting of the trauma in a safe, clinical setting. Eye-Movement Desensitization and Reprocessing (EMDR) is another effective treatment, in which patients recount traumatic events while following the therapist's hand movements or eye motions.
Pharmacological Treatment
Antidepressants are the preferred initial class of medications for PTSD. Selective Serotonin Reuptake Inhibitors (SSRIs) are the most commonly used, with sertraline and paroxetine being the only drugs approved by the FDA for PTSD treatment. Other options include serotonin-norepinephrine reuptake inhibitors (e.g., venlafaxine), tricyclic antidepressants, and monoamine oxidase inhibitors. Prazosin, an alpha-1 receptor blocker, has been found effective in reducing nightmares in PTSD patients.
Challenges and Barriers
One challenge in treating Afghanistan veterans with PTSD is the social stigma associated with mental illness within military communities. This stigma can lead to embarrassment and shame, causing veterans to avoid seeking treatment. Additionally, there is a shortage of mental health professionals in many parts of the US, particularly in rural areas, creating barriers to accessing care.
Future Directions
There is a need for more effective pharmacological treatments for PTSD, as not all patients respond adequately to existing drug therapies. Research is exploring the role of neurotransmitters like GABA and glutamate in encoding fear memories, which may open new avenues for treatment.
Telehealth, or the use of telecommunications technology to provide behavioral health services, is being utilized to improve access to care, especially for veterans in rural areas.
To support community-based mental health providers who may not be well-equipped to treat veterans with PTSD, the VA has developed the PTSD Consultation Program for Community Providers, offering education, training, and resources.
The Opiate Trail: Uncovering the Path of Afghan Opium to America's Streets
You may want to see also

PTSD symptoms and their intensity
Intrusion
PTSD is often characterised by involuntary and vivid reliving of the traumatic event, including repetitive and distressing images, sensations, and physical sensations such as pain, sweating, nausea, or trembling. Flashbacks may be so vivid that people feel they are reliving the traumatic experience or seeing it before their eyes. Nightmares and distressing dreams are also common.
Avoidance
People with PTSD may avoid reminders of the traumatic event, including people, places, activities, objects, and situations that may trigger distressing memories. They may try to avoid thinking about the event or talking about it. This can lead to feelings of isolation and emotional numbness.
Alterations in cognition and mood
People with PTSD may experience negative thoughts and feelings, such as guilt, shame, or distorted beliefs about themselves or others. They may also have ongoing fear, anger, or sadness, and may lose interest in activities they previously enjoyed. They may feel detached or estranged from others and have difficulty experiencing positive emotions.
Alterations in arousal and reactivity
PTSD can cause people to be easily startled, irritable, and have angry outbursts. They may be overly watchful of their surroundings and have difficulty concentrating or sleeping. Arousal symptoms can be constant and interfere with daily life.
Intensity and Duration
The intensity and duration of PTSD symptoms can vary widely between individuals. While some people experience long periods when their symptoms are less noticeable, others have constant severe symptoms. Symptoms usually develop during the first month after a traumatic event, but there may be a delay of months or even years before symptoms appear.
PTSD symptoms must last for more than a month and be severe enough to interfere with daily life, such as relationships or work, to meet the diagnostic criteria for PTSD. While some people recover within 6 months, others have symptoms that last for a year or longer.
Factors Affecting Intensity
The intensity of PTSD symptoms can be influenced by various factors, including the nature of the traumatic event, biological factors such as genes, and social support after the event. Previous traumatic experiences, particularly during childhood, can increase the likelihood of developing more intense PTSD symptoms.
PTSD in Specific Populations
The intensity and duration of PTSD symptoms can also vary among different populations. For example, combat veterans are at a much higher risk of experiencing PTSD than the general population, with rates ranging from 15% to 30% in some studies. Women are twice as likely as men to develop PTSD, possibly due to a higher risk of experiencing sexual trauma. PTSD in children may include re-enacting the traumatic event during play, bed-wetting, and thumb-sucking.
Medical Testing Procedures in Kabul, Afghanistan: Understanding the Timeline
You may want to see also

PTSD relapse and recurrence among Afghanistan veterans
Post-traumatic stress disorder (PTSD) is a debilitating anxiety disorder that occurs after a terrifying event. Military personnel, especially those involved in combat, are at an increased risk of developing the disorder. The condition affects as many as 40% of service members.
PTSD relapse and recurrence
The terms "relapse" and "recurrence" refer to the return of symptoms after a period of treatment. Relapse refers to the return of symptoms associated with a treated episode, while recurrence refers to the onset of a new episode. Unfortunately, there is limited research on the long-term effects of treatment for combat-related PTSD among veterans of Iraq and Afghanistan.
Studies on PTSD relapse and recurrence
A systematic review by Berge et al. (2020) identified only eight studies that examined relapse and recurrence rates among veterans of Iraq and Afghanistan. The majority of these studies were found to be at high risk of attrition bias, and few comprehensively reported relevant outcome statistics.
The included studies had small sample sizes, ranging from 26 to 268 participants. Most participants were male, and all met the diagnostic criteria for PTSD. The studies used various forms of exposure therapy or cognitive processing therapy as treatments.
Only one study reported rates of remission, clinically meaningful change, and loss of diagnosis at both post-treatment and follow-up. This study utilized a waitlist control group and found a slight decrease in all three measures at the last follow-up assessment. However, the lack of a control group in other studies makes it difficult to compare outcomes.
Factors affecting relapse and recurrence
Several factors may influence the relapse and recurrence of PTSD among Afghanistan veterans. These include the intensity and duration of the trauma, the presence of other mental health disorders, and the effectiveness of treatment. Additionally, high dropout rates from treatment and loss of follow-up data can impact the ability to assess long-term outcomes.
Recommendations for future research
The limited number of studies and their methodological shortcomings highlight the need for more rigorous research on PTSD relapse and recurrence among Afghanistan veterans. Future studies should aim for larger sample sizes, longer follow-up periods, and more consistent reporting of outcome measures. Additionally, the development of standardized definitions of relapse and recurrence would improve the quality of research in this area.
While PTSD is a significant issue among Afghanistan veterans, there is a lack of comprehensive research on relapse and recurrence rates. Further studies with improved methodologies are needed to better understand the long-term effects of treatment and to develop more effective interventions for this vulnerable population.
Marines' Extended Tours: The Afghanistan Story
You may want to see also

PTSD triggers in news and media
The news and media can be a source of PTSD triggers, especially for those who have experienced trauma first-hand. Below are some ways in which news and media coverage can act as a trigger for PTSD symptoms.
Graphic and Violent Content
The easy accessibility of graphic and violent content online, especially on social media, can be a source of PTSD triggers. A study by Dr Pam Ramsden of the University of Bradford found that more than a fifth of respondents scored high on clinical measures of PTSD from seeing pictures on social media—despite not having experienced the traumatic events themselves. The study suggested that the lack of warning or context before disturbing content on social media, as opposed to traditional media, could be a contributing factor.
Repeated Viewing
Repeated viewing of traumatic content can also increase the risk of developing PTSD symptoms. This is particularly relevant for individuals who may have experienced trauma first-hand, such as combat veterans, as they may be more susceptible to the effects of repeated exposure.
24-Hour News Cycles and Sensationalism
The constant availability of news and the sensationalist nature of 24-hour news cycles can contribute to PTSD symptoms. This is especially true for social media, which often contains more graphic and disturbing images than traditional news sources. The pervasiveness of social media and around-the-clock news coverage increases the likelihood of exposure to potentially traumatic content.
Lack of Context
Media coverage that lacks context, such as failing to provide a broader understanding of an issue or event, can also trigger PTSD symptoms. For example, children may struggle to process traumatic news without the appropriate context and may need additional support to understand and cope with what they are seeing and hearing.
Individual Factors
Individual factors, such as pre-existing mental health conditions or previous trauma exposure, can also influence the impact of media exposure on PTSD symptoms. Some individuals may be more susceptible to developing PTSD symptoms due to biological or neurobiological factors that influence their response to stress and traumatic events.
Impact on Children and Adolescents
Children and adolescents are particularly vulnerable to the effects of media exposure on their mental health. Research has shown that exposure to disaster-related news coverage and social media apps can trigger post-traumatic stress symptoms in young people, even if they are not directly affected by the events. This is of particular concern given the increasing frequency of climate-related disasters and the widespread use of social media among young people.
**A World Away: The Distance Between Yemen and Afghanistan**
You may want to see also
Frequently asked questions
Post-Traumatic Stress Disorder (PTSD) is a mental health condition characterised by persistent emotional and mental distress after witnessing or experiencing a terrifying event.
Studies suggest that between 10% and 40% of veterans suffer from PTSD.
The core symptoms of PTSD are persistent re-experiencing of the trauma, avoidance of trauma-related stimuli, negative alterations in cognition and mood, and increased arousal and reactivity.
Treatments for PTSD include cognitive processing therapy, prolonged exposure therapy, virtual reality exposure therapy, and eye movement desensitization and reprocessing (EMDR).







